Did you know that the leading cause of blindness and vision impairment in working-age Americans is from diabetes? Diabetic Retinopathy is the most prevalent and visually significant disease of the eye in this group of patients. It affects both Type 1 and Type 2 diabetics. According to the CDC, from 2010 to 2050, the number of Americans with diabetic retinopathy is expected to nearly double, from 7.7 million to 14.6 million. It’s important to know the signs and take an active role in managing diabetes because, with early detection and proper care, permanent vision loss can be prevented. Below are some of the most common questions and answers we discuss with patients:
How can diabetes affect your vision?
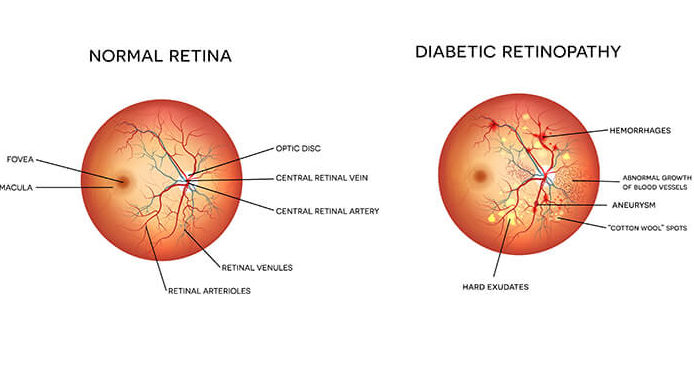
Diabetes is a condition that causes damage to the vasculature, or the blood vessels in the body, including the eye. When these blood vessels in the eye become weak, they begin to leak fluid and sometimes bleed, which can permanently damage your retina (the light-sensitive tissue in the back of your eye), resulting in vision loss.
What are the symptoms?
Much like high blood pressure, diabetic retinopathy may not have any noticeable symptoms in the early stages. This is why it’s so important to get a dilated eye exam each year and to have your blood glucose levels and Hemoglobin A1c levels routinely monitored by your primary care physician. Some noticeable symptoms that may arise at later stages include:
- Blurry Vision
- Early formation of and/or rapid progression of cataract
- Poor color contrast
- Glare (especially with nighttime vision)
- Halos
- Floaters (when bleeding has occurred)
- Loss of vision
Once there is damage to the eye from diabetic retinopathy, is it treatable or reversible?
The primary and most important prevention, as well as the treatment of diabetic eye disease, is good blood sugar control. If problems do begin to occur, catching the disease early is key. If it is treated early enough, it is possible to reverse diabetic changes in the eye. The initial stage is called Background Diabetic Retinopathy. In this stage, lasers may be used to treat fluid accumulation in the retina which may be affecting vision. As the disease progresses into what is called Proliferative Diabetic Retinopathy, injections in the eye may be required, in addition to further laser treatments, as there are significantly more fluid and bleeding accumulating. It is possible that scar tissue will begin to develop that may cause permanent damage to the eye. Unfortunately, once the retinal tissue begins to scar significantly, damage to the tissue as well as the resolution of symptoms may become irreversible.
What’s the best way to prevent diabetic eye disease?
- Blood sugar must be monitored very closely and remain stable within a healthy range.
- Ensure hemoglobin A1C is regularly checked and remains in a good range.
- Attend your dilated eye exam with your eye care provider each year to safeguard yourself against permanent vision loss.

Written By: Dr. Matthew Smith, MD
Dr. Matthew Smith is a board-certified ophthalmologist at the Williamson Eye Center. Dr. Smith specializes in the treatment of glaucoma, glaucoma surgery, and both cataract and refractive surgery.